The 5 Most Common Hand Injuries We Treat (and How We Help)
There is an infinite amount of injuries that can occur in the upper extremity. With experience in the ortho OT practices, as well as PT practices, certain injuries appear again and again. Of course, there are the common repetitive strain conditions, such as carpal tunnel syndrome or cubital tunnel syndrome, but I wanted to talk about some common traumatic injuries that happen and how we deal with these. Understanding their typical course can ease anxiety and set realistic expectations.
Distal Radius Fracture
Often from a fall on an outstretched hand. This is one of the forearm bones that, after a fall, breaks right near the wrist. Instead of the wrist wanting to bend, the radius gives way. The most common of the distal radius fractures is a Colles fracture, where the fractured part of the bone moves dorsally. Regardless of if it was displaced (needing realignment) or non-displaced (fractured but still in good alignment), early finger motion and swelling control are followed by progressive wrist strengthening once the cast is removed.
We can’t just move straight into strengthening, though. After the cast is removed, we need to make sure range of motion is restored. Timewise, the cast can come off sooner if hardware was placed to keep the bones in alignment vs. trying to allow the bone to heal by secondary healing (on its own). This would be in 3 planes: flexion/extension, ulnar/radial deviation, and supination/pronation. If we are diligent with early finger motion and swelling control, we won’t have to worry about the fingers as much, and the outcomes for the wrist will actually be better too. Once range of motion is trending in the right direction, then progressive strengthening can be initiated.
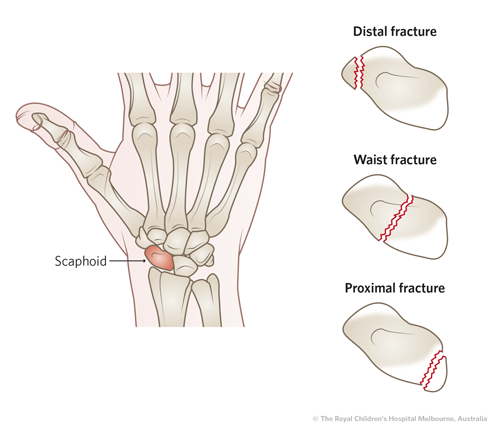
Scaphoid Fracture
A small bone in the wrist with limited blood supply. This would be another wrist fracture, which is often misdiagnosed because it is hard to see in certain angles of X-Rays. I actually had a friend who fell off his bike on an outstretched hand, went to urgent care, and the X-Ray showed no fractures, so they assumed he must have just sprained it. (Well, certain sprains can also be quite serious in the wrist, but that is for another time). He went about his life for many weeks with his wrist in pain until his wife had me check it out. Upon examination and palpating the scaphoid bone with quite a sudden pain response, I told my friend that he should probably see a doctor about it because he probably broke this bone. Sure enough, the next X-Ray by an orthopedic doctor confirmed the scaphoid fracture. This type of story is common.
Custom thumb‑spica splints and cautious loading prevent non‑union and long‑term stiffness. Luckily for my friend, despite lack of care for the first few weeks, his scaphoid bone did heal. Due to poor blood supply to this bone, people are at risk for non or mal-union, which can pose long term problems such as arthritis or wrist kinematic issues. All goes to say, if we can get a proper diagnosis and treat the hand early on with appropriate splinting and early mobilization, outcomes will be optimal and return to sport (like cycling for my friend) or activity will be more likely.
Mallet Finger
A fingertip that will not straighten after a sudden force, or extreme over stretching of the dorsal side of the fingertip. For example, I recently had a patient who played football for school. The ball happened to hit his fingers on the backside of his hand in the wrong way during a pass, and left his finger drooped and completely swollen. X-Ray showed he had fractured the distal phalanx right where his tendon attaches to the bone.
Apart from sudden force, let’s talk about extreme stretching. There is the bony mallet finger (the football player), and there is also a soft tissue mallet finger, where the bone remains intact, but the tendon/soft tissue becomes overstretched. Another friend I swim with, one day, was attempting to don his wetsuit. Wetsuits are the bane of my existence! I understand their purpose, but they are so dang difficult to put on if they are well fitting. With the strong gripping of this wetsuit, my friend suddenly noticed that his finger could not straighten. It wasn’t blunt force, but just a little overly prolonged gripping and friction from the wetsuit that caused this zone 5 extensor tendon injury. Beware of the wetsuit. Continuous splinting for 6-8 weeks, then safe and progressive mobilization, yields excellent results when started promptly.
PIP Joint dislocation
We will get a PIP Joint dislocation also from sudden force, or from falling. With dislocations, we want to be careful and communicate with the doctor and patient on exact mechanism of injury, which will dictate how treatment goes subsequently. If we have a dorsal dislocation, for example, we will not be splinting the finger straight. In fact, we will have to immobilize that joint in slight flexion, due to the overstretching and injury of the volar plate. On the other hand, a volar dislocation would result in splinting the PIP joint in full extension, so that the central slip can scar and shorten properly. It is important to communicate with the doctor because we need to know how much of the tendon was injured, if at all, and if the lateral bands were involved.
If a more mild grade, perhaps what you need are some buddy loops. All sorts of things can happen with dislocations, and it’s not always just in one direction (it could have dislocated sideways). So the treatment for this can be variable. Bottom line is we want to know how the dislocation happened because that will govern what we do next.
Thumb UCL tear
Overstretching or tear of one of the collateral ligaments of the thumb metacarpophalangeal joint. Again, it is still really important to get this injury checked out by a hand surgeon or orthopedic doctor because depending on the level of tear, you may need surgery. Sometimes the tear happens at the point where the thumb adductor also attaches, in which case conservative healing will not happen.
Conservative or post-op, we’ll need to make a custom thumb spica, in order to heal and scar that area in proper alignment. As mobilization is approved to start, we would continue to protect the ulnar collateral ligament (UCL) by moving the thumb in the sagittal plane to the hand, until ready to move on to other thumb rotational planes. Then progressive strengthening.
Call for a free consultation and screening
Facing any of these injuries? The sooner therapy begins, the smoother the outcome. Schedule a consultation at Reach Beyond Therapy to start a proven path back to full function. 323-844-8450 or email me so we can connect jade@reachbeyondtherapy.com